Overview
The article outlines five essential checkpoints for individuals experiencing persistent hunger while using Ozempic. These checkpoints focus on:
- Dosage evaluation
- Dietary adjustments
- Sleep quality
- Physical activity
- Emotional well-being
Each checkpoint is accompanied by practical advice:
- Consulting healthcare providers for effective dosage management
- Incorporating high-protein and fiber-rich foods into meals
- Ensuring adequate sleep
- Engaging in regular exercise
- Monitoring emotional triggers to foster healthier eating habits
This structured approach not only addresses the immediate concerns of hunger but also encourages a holistic view of health management.
Introduction
Navigating the journey of weight loss while using Ozempic often presents unexpected challenges, particularly when hunger pangs persist despite the medication’s intended effects. Understanding how to effectively manage these hunger signals is crucial for achieving sustainable results. This article explores five essential checkpoints that can assist individuals in fine-tuning their approach. It addresses key areas such as:
- Dosage evaluation
- Dietary adjustments
- Sleep quality
- Physical activity
- Emotional well-being
How can one ensure that their weight loss efforts remain on track while still experiencing hunger on Ozempic?
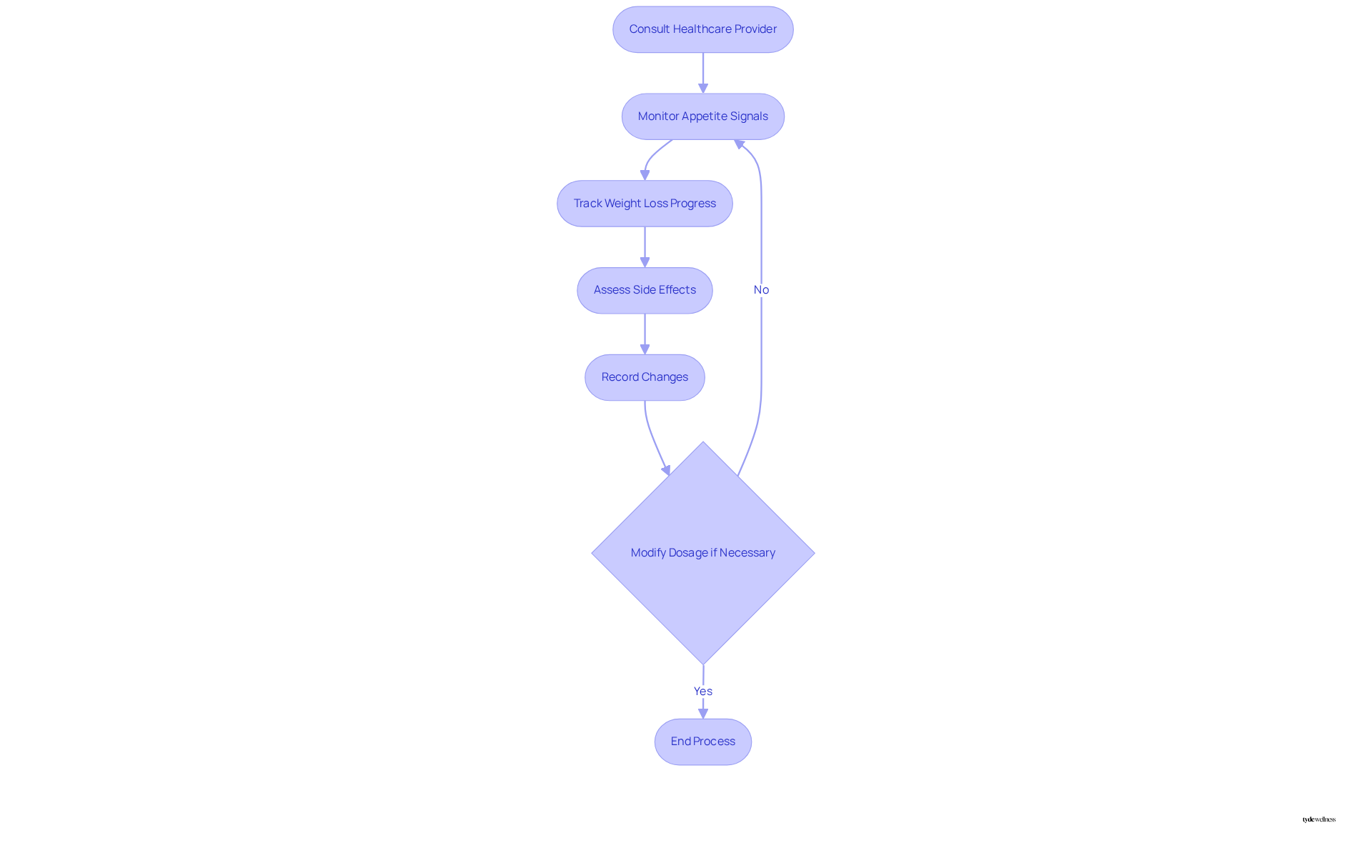
Evaluate Your Dosage of Ozempic
- Consult your healthcare provider to assess your current Ozempic dosage and its effectiveness in managing your appetite levels, as professional oversight is essential before making any adjustments.
- Regularly monitor your appetite signals and track your weight loss progress to identify if dosage adjustments are necessary. Be aware that common side effects of Ozempic, such as nausea and vomiting, may occur when starting or increasing the dosage, which might make you still hungry on Ozempic.
- The typical starting dose of Ozempic is 0.25 mg, which can be increased based on individual response and needs, often reaching up to 1 mg or more as required.
- Keep a thorough record of your appetite signals and any alterations in your eating habits to enable a constructive conversation with your healthcare provider.
Real-life examples demonstrate that individuals may need to modify their Ozempic dosage to better control appetite, particularly if they find themselves still hungry on Ozempic, ensuring that their weight loss journey remains effective and sustainable. Participants in the Tyde Wellness program have reported an average body mass loss of 15% after 68 weeks, highlighting the significance of customized dosage adjustments.
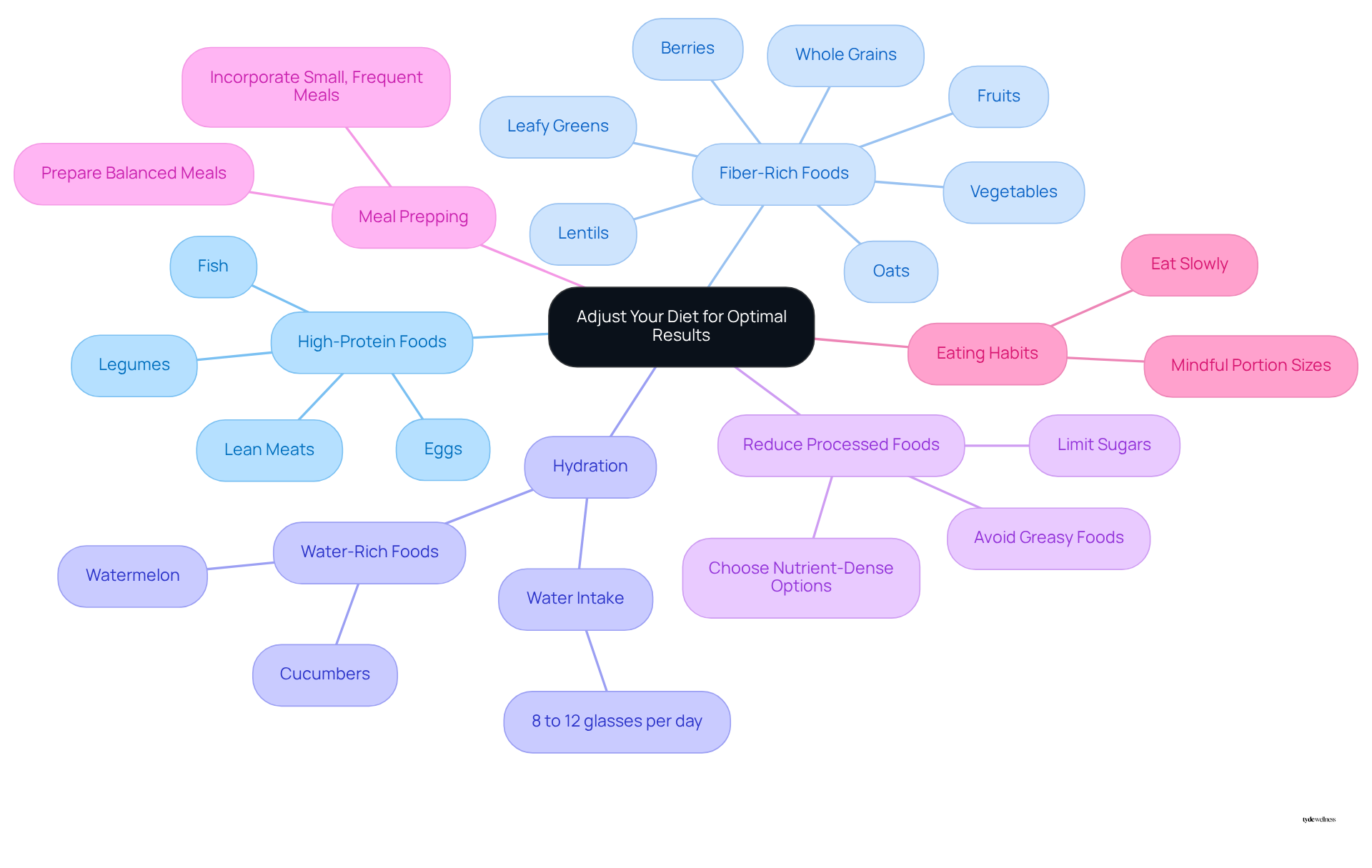
Adjust Your Diet for Optimal Results
- Incorporate high-protein foods such as lean meats, fish, eggs, and legumes into your meals. These foods support muscle maintenance and enhance satiety. Aim for 20 to 30 grams of protein at the start of every meal to maximize fullness and reduce cravings.
- Focus on fiber-rich foods like vegetables, fruits, and whole grains. These are essential for promoting fullness and preventing constipation, especially for those who are still hungry on Ozempic, a common side effect of GLP-1 medications. Good sources of fiber include oats, berries, leafy greens, and lentils.
- Drink 8 to 12 glasses of water per day. This helps manage dehydration and constipation associated with GLP-1 medications.
- Reduce processed foods and sugars, as they can increase appetite and worsen nausea and discomfort, hindering your weight loss efforts. Instead, choose nutrient-dense options.
- Consider meal prepping to ensure you have healthy options readily available. Preparing balanced meals in advance can help you stick to your dietary goals. This approach makes it easier to incorporate small, frequent meals that align with your body’s needs when you are still hungry on Ozempic. Aim for a balanced plate consisting of half fruits and vegetables, one-quarter protein, and the rest whole grains.
- Eat slowly to allow your brain to register fullness, which helps avoid overeating.
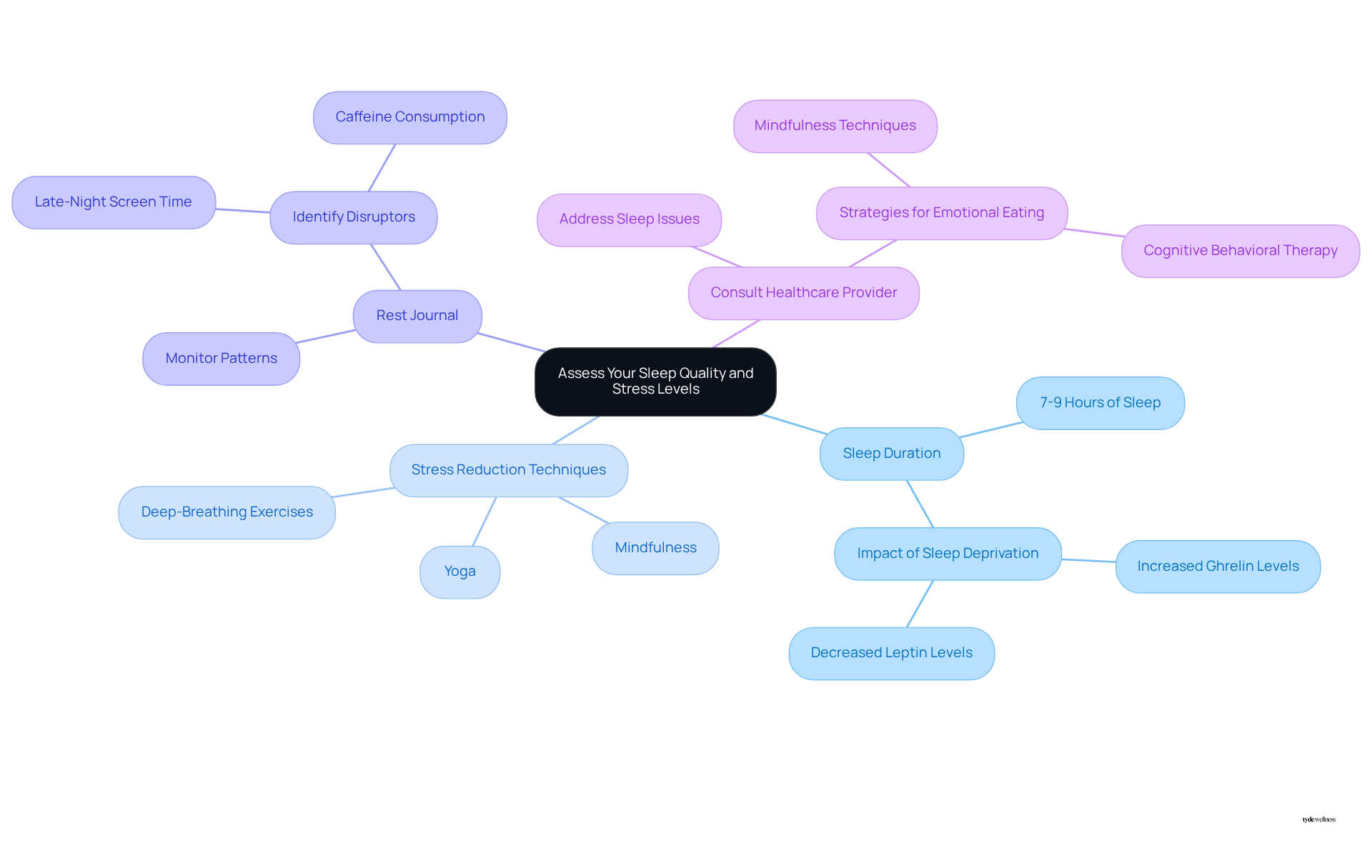
Assess Your Sleep Quality and Stress Levels
- Strive for 7-9 hours of restorative rest each night, as adequate relaxation is essential for managing hormones that influence appetite and metabolism. Research indicates that individuals who rest for fewer than six hours are more prone to gaining weight compared to those who rest for seven to eight hours. This is attributed to hormonal imbalances, particularly elevated ghrelin levels, which increase appetite, and reduced leptin levels, which signal satiety.
- Implement stress-reduction techniques such as mindfulness, yoga, or deep-breathing exercises. These methods not only alleviate stress but also help manage emotional eating, which can be exacerbated by insufficient rest. Dr. Audrey Wells emphasizes the connection between rest and eating habits, noting that stress can lead to cravings for high-calorie foods. She states, ‘When you go in and manipulate one of those, it’s not surprising that the other is affected.’
- Maintain a rest journal to monitor patterns and identify factors that influence your quality of rest. This practice can help pinpoint issues such as late-night screen time or caffeine consumption that may disrupt your sleep. Establishing a consistent rest pattern can enhance your body’s response to weight management therapies like Semaglutide.
- Consult with a healthcare provider if sleep issues persist. A doctor specializing in weight loss can recommend strategies to address emotional eating and improve sleep practices, ensuring that your weight reduction journey remains on track. Addressing sleep-related challenges is vital for maximizing the effectiveness of weight loss medications and achieving sustainable results.
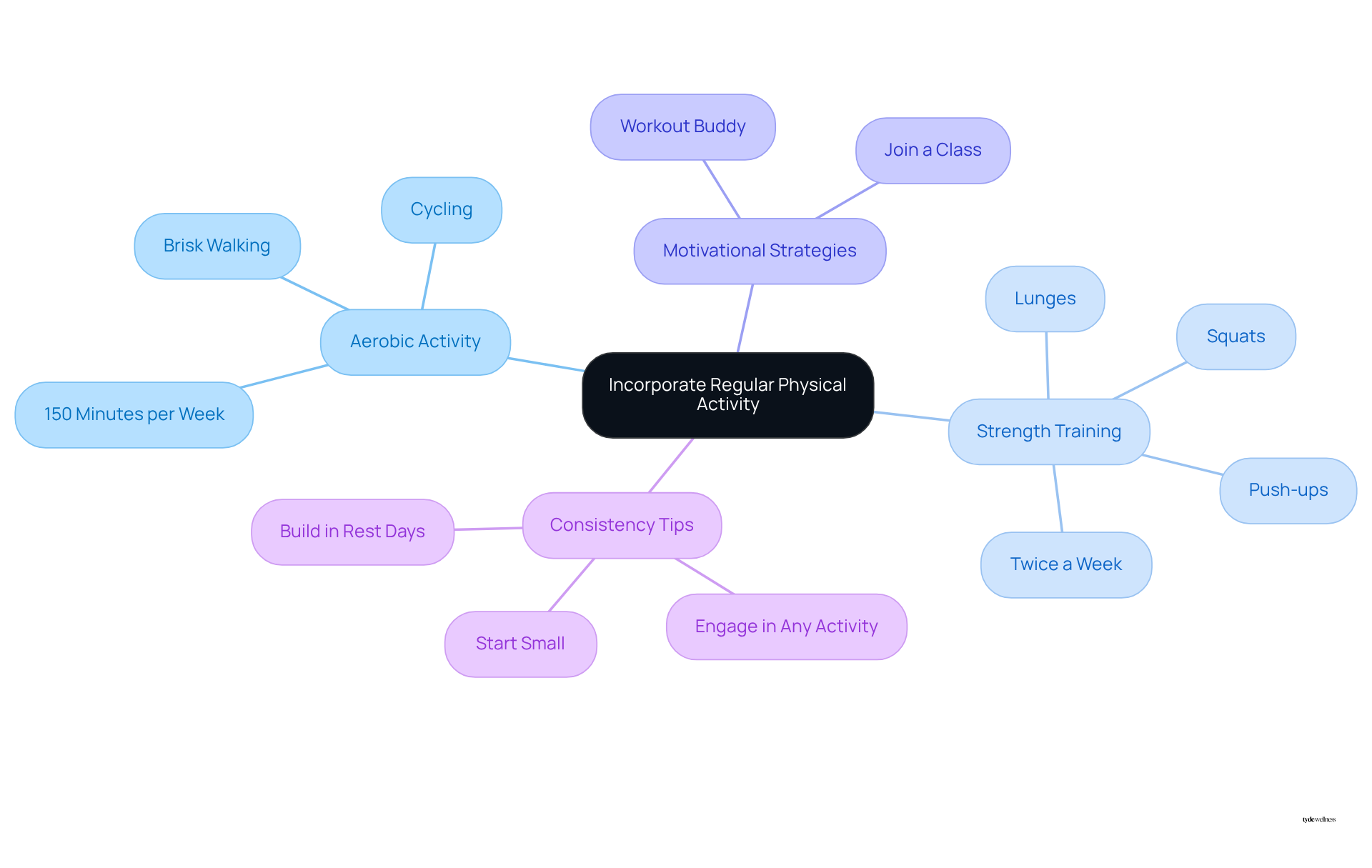
Incorporate Regular Physical Activity
Aim for at least 150 minutes of moderate-intensity aerobic activity each week, such as brisk walking or cycling. This supports cardiovascular health and aids in weight management. Incorporate strength training exercises at least twice a week, focusing on movements like squats, lunges, and push-ups. These exercises help build muscle and boost metabolism.
Choose activities that you genuinely enjoy, as this approach makes it easier to integrate exercise into your daily routine and maintain consistency. Furthermore, consider joining a fitness class or partnering with a workout buddy. This can enhance motivation and accountability, making your exercise journey more enjoyable.
Remember that even on days when motivation is low, engaging in any form of physical activity is beneficial. Doing something active, such as walking or climbing stairs on rest days, can positively contribute to your routine. Starting small, like with 10 minutes of stationary bike riding daily, can lead to significant long-term results.
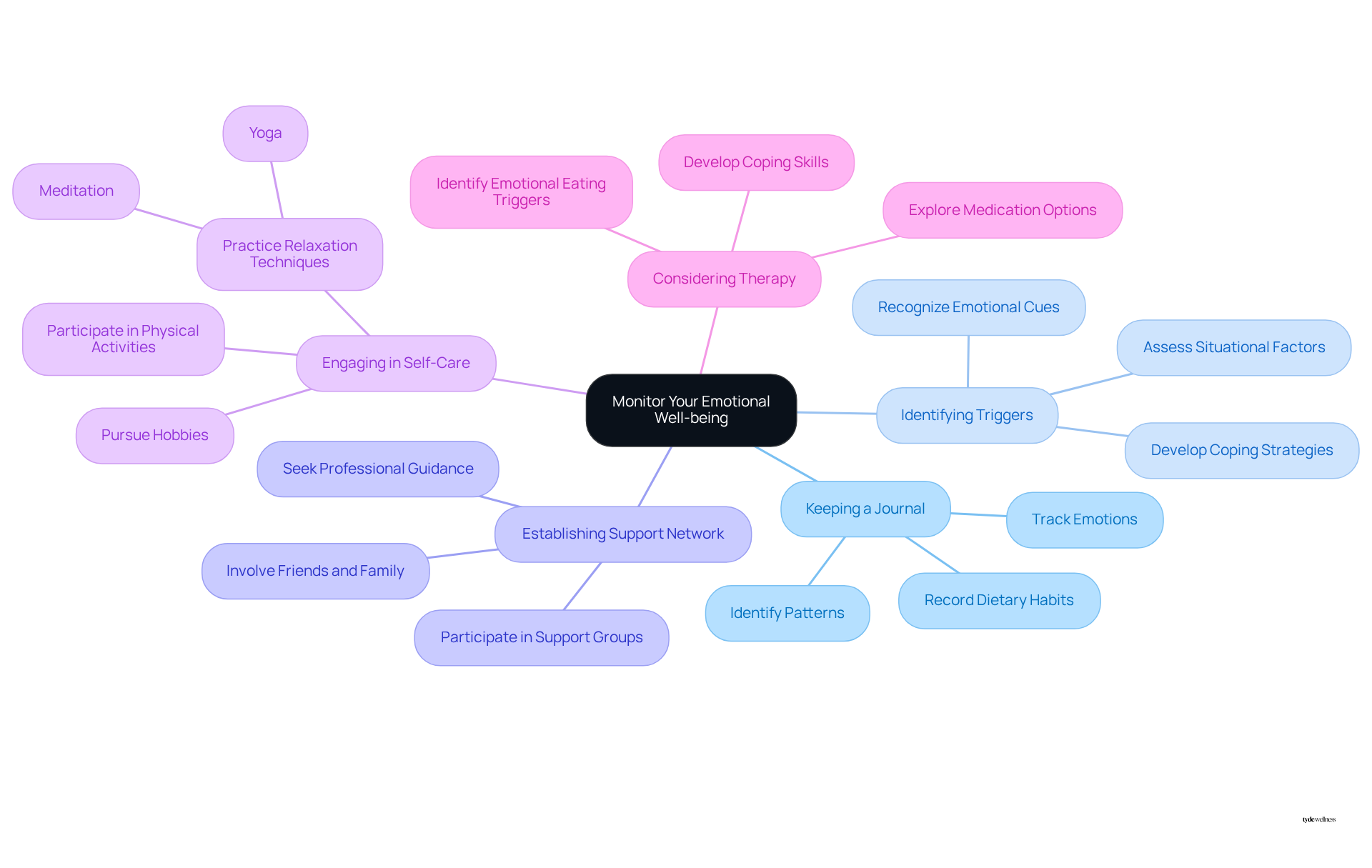
Monitor Your Emotional Well-being
- Keeping a journal can effectively monitor your emotions and dietary habits. Research indicates that emotional consumption often leads to excessive intake, driven by feelings rather than physical appetite. This practice aids in distinguishing between emotional and physical hunger, thereby promoting healthier dietary habits.
- Identifying emotional triggers that may lead to unhealthy consumption behaviors is crucial. This awareness enables proactive management of such situations, reducing the likelihood of emotional eating.
- Establishing a support network of friends, family, or mental health professionals is beneficial for discussing challenges and seeking guidance when needed. A strong support system can significantly decrease the chances of succumbing to emotional consumption.
- Engaging in self-care practices that enhance emotional well-being is essential. Activities such as pursuing hobbies, practicing relaxation techniques like yoga or meditation, and participating in physical exercises can foster a healthier mindset.
- Considering therapy as a valuable tool for managing emotional eating can be effective. Therapy can help individuals identify triggers and develop coping strategies that promote healthier eating behaviors.
Conclusion
Managing hunger while on Ozempic necessitates a multifaceted approach that addresses various elements of health and lifestyle. Evaluating dosage, adjusting dietary habits, ensuring quality sleep, incorporating regular physical activity, and monitoring emotional well-being are essential for enhancing the experience with Ozempic and effectively supporting weight loss efforts.
Key strategies involve:
- Consulting healthcare providers for dosage assessments
- Prioritizing high-protein and fiber-rich foods
- Maintaining proper hydration
- Establishing a consistent sleep routine
- Engaging in stress-reduction techniques
These strategies can significantly influence appetite regulation. Physical activity, tailored to personal preferences, not only aids in weight management but also contributes to overall well-being.
Ultimately, addressing hunger on Ozempic requires a holistic approach that encompasses medical guidance, dietary adjustments, emotional health, and lifestyle changes. By implementing these strategies, individuals can manage their hunger more effectively and pave the way for sustainable weight loss and improved health outcomes. Taking proactive steps toward these goals can lead to a more fulfilling and successful journey with Ozempic.
Frequently Asked Questions
How should I evaluate my dosage of Ozempic?
Consult your healthcare provider to assess your current Ozempic dosage and its effectiveness in managing your appetite. Regular monitoring of your appetite signals and weight loss progress is important to determine if dosage adjustments are necessary.
What is the typical starting dose of Ozempic?
The typical starting dose of Ozempic is 0.25 mg, which can be increased based on individual response and needs, often reaching up to 1 mg or more as required.
What common side effects should I be aware of when taking Ozempic?
Common side effects of Ozempic include nausea and vomiting, which may occur when starting or increasing the dosage. These side effects might contribute to feelings of hunger while on Ozempic.
How can I track my progress while using Ozempic?
Keep a thorough record of your appetite signals and any changes in your eating habits. This information will help facilitate a constructive conversation with your healthcare provider regarding any necessary dosage adjustments.
What dietary adjustments can enhance the effectiveness of Ozempic?
Incorporate high-protein foods (like lean meats, fish, eggs, and legumes) into your meals, aiming for 20 to 30 grams of protein at the start of each meal. Focus on fiber-rich foods (such as vegetables, fruits, and whole grains) to promote fullness and prevent constipation.
How much water should I drink daily while on Ozempic?
It is recommended to drink 8 to 12 glasses of water per day to help manage dehydration and constipation associated with GLP-1 medications like Ozempic.
What types of foods should I reduce or avoid while on Ozempic?
Reduce processed foods and sugars, as they can increase appetite and worsen nausea and discomfort, which may hinder your weight loss efforts. Instead, opt for nutrient-dense options.
How can meal prepping help with my dietary goals on Ozempic?
Meal prepping ensures you have healthy options readily available, making it easier to stick to your dietary goals. It allows you to incorporate small, frequent meals that align with your body’s needs, especially when experiencing hunger on Ozempic.
What is a balanced plate composition for meals?
Aim for a balanced plate consisting of half fruits and vegetables, one-quarter protein, and the rest whole grains to support your dietary goals.
How can I avoid overeating while on Ozempic?
Eat slowly to allow your brain to register fullness, which helps prevent overeating.
List of Sources
- Evaluate Your Dosage of Ozempic
- Ozempic for Weight Loss: Does It Work and Is It Safe? – GoodRx (https://goodrx.com/ozempic/ozempic-for-weight-loss?srsltid=AfmBOooW2_mM6GiH2bmCxRtBm33VmA2evy_S_Vfi72bLXFy-5KGKuH8X)
- Ozempic dosage: Form, strengths, how to use, and more (https://medicalnewstoday.com/articles/drugs-ozempic-dosage)
- Ozempic Dosing Guide: Overdose, Strengths, Forms, and More (https://healthline.com/health/drugs/ozempic-dosage)
- Dosing Schedule | Ozempic® (semaglutide) injection (https://ozempic.com/how-to-take/ozempic-dosing.html)
- Ozempic vs Wegovy, Mounjaro and Zepbound: A comprehensive guide (https://northwell.edu/news/insights/ozempic-for-weight-loss-does-it-work)
- Adjust Your Diet for Optimal Results
- 7 Types of Foods and Drinks to Avoid When Taking Ozempic or Wegovy for Weight Loss (https://today.com/health/diet-fitness/ozempic-foods-to-avoid-rcna101369)
- Many people using GLP-1 weight loss drugs may not be eating enough nutritious food (https://uchealth.org/today/nutrition-vital-when-taking-glp-1-weight-loss-drugs)
- ‘Ozempic Diet’: Foods to Eat and Avoid on a GLP-1 Obesity Drug (https://webmd.com/obesity/features/ozempic-diet-foods)
- 5 things doctors want you to know before you start taking a GLP-1 (https://washingtonpost.com/wellness/2025/07/15/glp1-ozempic-nutrition-muscle-loss)
- Ozempic: Increasing Protein Intake Could Help Prevent Muscle Loss (https://healthline.com/health-news/protein-muscle-loss-weight-loss-drugs)
- Assess Your Sleep Quality and Stress Levels
- How Sleep Quality and Duration Influence Your Weight Loss Goals (https://drfortino.net/blog/how-sleep-quality-and-duration-influence-your-weight-loss-goals)
- The Connection Between Sleep, Diabetes, and Obesity (https://yalemedicine.org/news/sleep-diabetes-and-obesity)
- Can Ozempic Impact Sleep? Social Media Study Finds Theme of Ozempic-Related Sleep Issues | Sleepopolis (https://sleepopolis.com/news/ozempic-sleep-related-issues-on-the-rise)
- Here’s How Weight Management Drugs May Impact Your Sleep (https://health.com/ozempic-sleep-apnea-8410283)
- Healthy Weight Control (https://newsinhealth.nih.gov/2022/12/healthy-weight-control)
- Incorporate Regular Physical Activity
- On Ozempic? Diet and Exercise are Still Key, Montclair Experts Say (https://montclair.edu/cchl/2024/09/10/on-ozempic-diet-and-exercise-are-still-key-montclair-experts-say)
- Ozempic: Exercise Is Still Vital for People Taking Anti-Obesity Drugs (https://healthline.com/health-news/exercise-important-while-taking-ozempic)
- People taking the new anti-obesity medications must make time for physical activity, say KU researchers (https://kumc.edu/about/news/news-archive/weight-loss-drugs-and-exercise.html)
- Monitor Your Emotional Well-being
- Tips to stop emotional eating (https://mayoclinic.org/healthy-lifestyle/weight-loss/in-depth/weight-loss/art-20047342)
- Ozempic & Emotional Eating: Breaking the Cycle of Stress and Food with Medication Support (https://betterucare.com/post/ozempic-emotional-eating-breaking-the-cycle-of-stress-and-food-with-medication-support)
- Anxiety fuels emotional eating and weight gain, study finds (https://news-medical.net/news/20250408/Anxiety-fuels-emotional-eating-and-weight-gain-study-finds.aspx)
- Emotional eating affects you and your child (https://news.sanfordhealth.org/parenting/emotional-eating-affects-you-and-your-child)
- Ozempic Hurts the Fight Against Eating Disorders (https://time.com/6966957/ozempic-eating-disorders-essay)


