Overview
The article titled “7 Steps to Get Semaglutide Covered by Insurance” primarily addresses how individuals can effectively secure insurance coverage for semaglutide treatment. It outlines essential steps, including:
- Consulting healthcare providers
- Verifying insurance coverage
- Submitting necessary documentation
- Navigating the appeal process for denied claims
The emphasis is on the importance of thorough preparation and a clear understanding of insurance policies, as these factors can significantly improve the likelihood of obtaining coverage for this medication.
Introduction
Navigating the complexities of insurance coverage for semaglutide can feel overwhelming, especially for those seeking effective weight loss solutions. With the rising demand for GLP-1 medications, understanding how to secure coverage is essential for individuals aiming to transform their health. This article provides a clear, step-by-step guide to help patients successfully obtain semaglutide through insurance. It addresses common challenges and offers valuable insights into:
- Eligibility criteria
- Documentation requirements
- The appeal process
What steps can one take to ensure they are informed and empowered in their pursuit of this potentially life-changing treatment?
Tyde Wellness: Personalized Weight Loss Programs with Semaglutide Coverage
Tyde Wellness offers that incorporate GLP-1 medication, specifically tailored for women experiencing significant life changes, including postpartum recovery and menopause. These programs focus on sustainable weight reduction strategies, allowing clients to achieve their health goals while navigating the complexities of medication payment options. By merging medical expertise with personalized nutrition plans, Tyde Wellness guarantees that each participant receives the essential support needed to succeed in their weight loss journey.
The effectiveness of GLP-1 medication in facilitating weight loss is particularly noteworthy. Research indicates that women often report higher success rates when utilizing GLP-1 therapies. This holistic approach not only addresses weight management but also promotes overall well-being, making it a valuable option for women pursuing lasting health transformations.
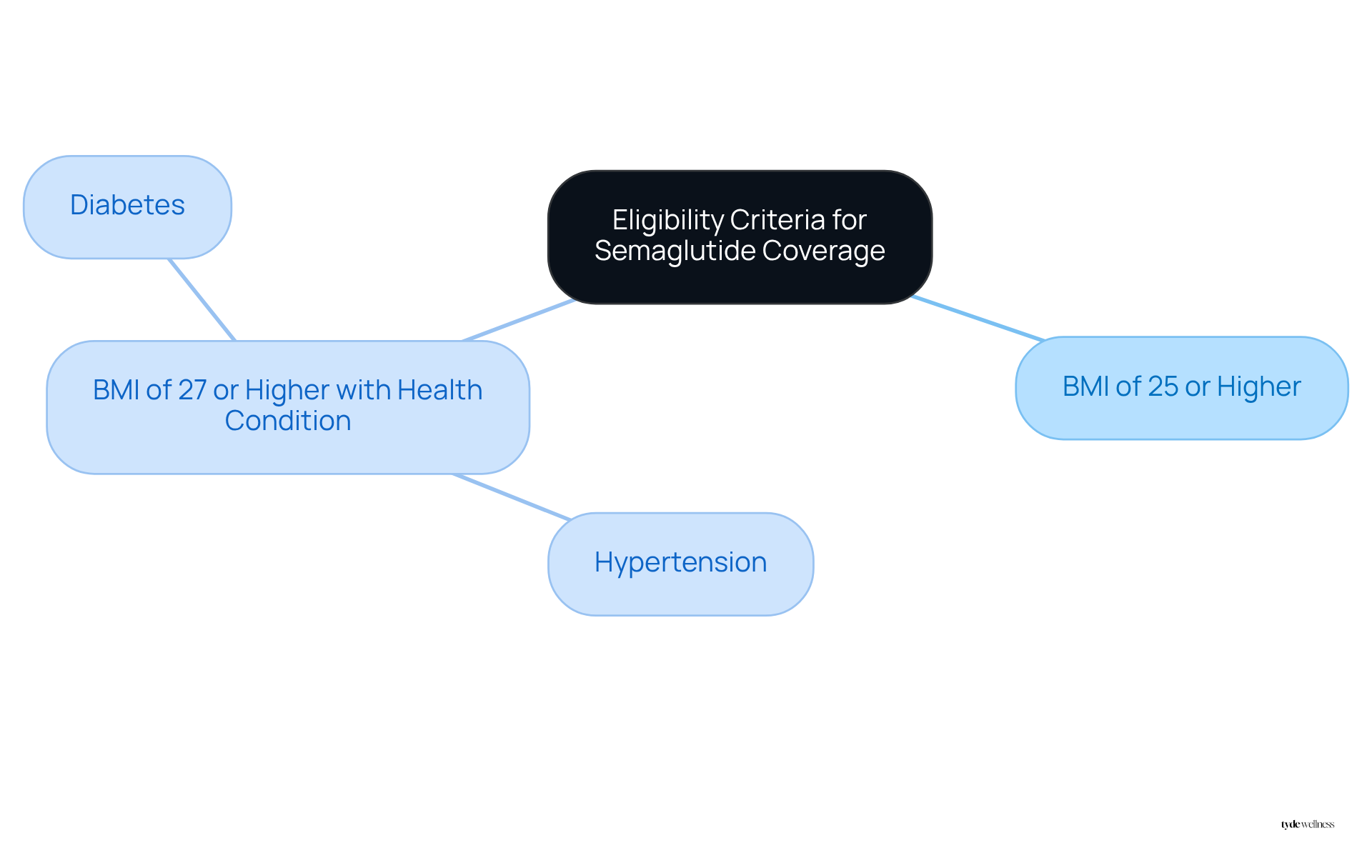
Understand Eligibility Criteria for Semaglutide Insurance Coverage
To qualify for medication coverage, individuals typically need to meet specific criteria. This often includes:
- Having a body mass index (BMI) of 25 or higher, or
- A BMI of 27 or higher accompanied by at least one weight-related health condition, such as hypertension or diabetes.
At Tyde Wellness, we adopt a personalized strategy for weight loss, evaluating each person’s health, goals, and lifestyle during the initial consultation. This customized approach not only aids in determining eligibility for GLP-1 therapy but also reflects our dedication to sustainable wellness.
Understanding these criteria is crucial for patients to and prepare for discussions with their healthcare providers. Furthermore, as part of the Tyde Circle, members are encouraged to connect with their communities, sharing insights and supporting one another in their weight loss journeys, which empowers women in their pursuit of health.
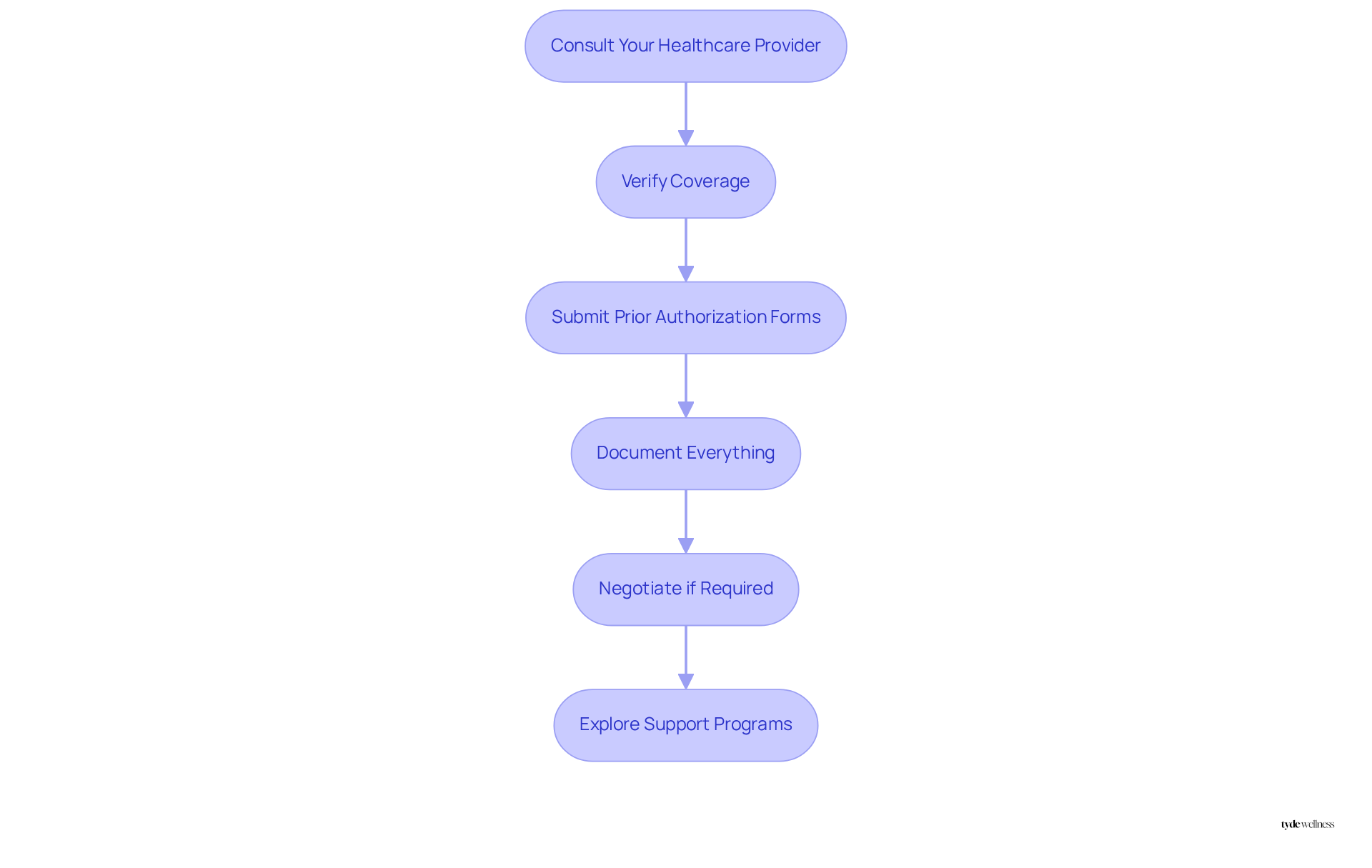
Follow Steps to Obtain Semaglutide Through Your Insurance
To successfully obtain semaglutide through insurance, follow these essential steps:
- Consult Your Healthcare Provider: Begin by discussing your need for the medication with your healthcare provider. They can evaluate your situation and provide a prescription if appropriate.
- Verify Coverage: Reach out to your provider directly or utilize their online resources to . This step is crucial, as coverage can vary significantly between different insurers and plans. Notably, only 45% of private health plans include coverage for this medication aimed at weight reduction, making it essential to comprehend the details of your plan.
- Submit Prior Authorization Forms: Ensure that your healthcare provider submits any required prior authorization forms to your coverage plan. This documentation is frequently required to demonstrate the medical necessity of the medication for your treatment.
- Document Everything: Keep meticulous records of all communications and documentation related to your request. This includes notes from conversations with your insurer and copies of any submitted forms, as these can be vital if you need to appeal a denial.
- Negotiate if Required: If your initial request is denied, don’t hesitate to discuss terms with your coverage provider. Examine your policy specifics and consider asking for a formal appeal, as numerous individuals have effectively reversed denials by proving the medical necessity of the treatment. As Dr. Vanessa Niles points out, protection will rely on the provider’s policies, personal plan, diagnosis, and medical history.
- Explore Support Programs: If medical benefits remain elusive, investigate assistance programs provided by manufacturers such as Novo Nordisk. These programs can offer semaglutide at lower prices or even free for qualifying individuals. For instance, a patient managed to acquire Ozempic at a reduced price through Novo Nordisk’s assistance program after her coverage only partially addressed it.
- Consult Insurance Experts: For further assistance, consider discussing with insurance professionals who can offer insights into maneuvering through the protection process. They can assist in clarifying your choices and recommend methods to enhance your likelihood of securing protection.
By following these steps, you can improve your chances of obtaining coverage for this effective treatment, making it more accessible.
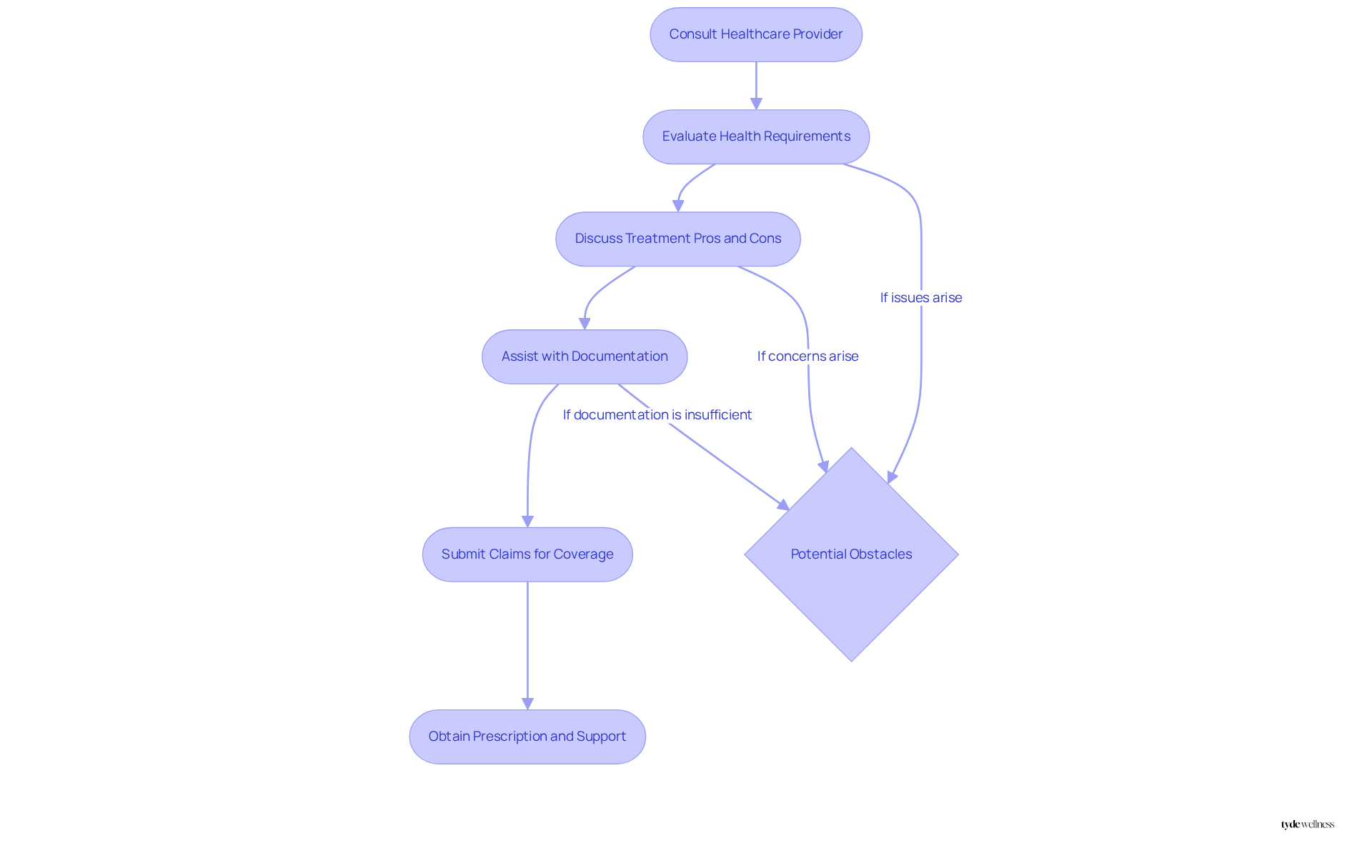
Consult Healthcare Providers for Semaglutide Prescription Guidance
Consulting with healthcare providers is essential for acquiring a prescription for medication. At Tyde Wellness, our skilled physicians and health coaches evaluate personal health requirements and discuss the potential advantages and drawbacks of treatment. They assist individuals through the often intricate coverage process, playing a crucial role in supplying the necessary documentation for claims. This significantly increases the chances of obtaining coverage for semaglutide.
With our customized peptide therapy and micro-dosed weight loss medications, along with , we ensure that individuals receive support that aligns with their weight management objectives. Appropriate documentation and comprehensive communication with providers can lead to improved outcomes. Many individuals may encounter obstacles due to high expenses and differing coverage policies.
Engaging with a knowledgeable provider not only streamlines the process but also empowers patients to make informed decisions about their weight management journey.
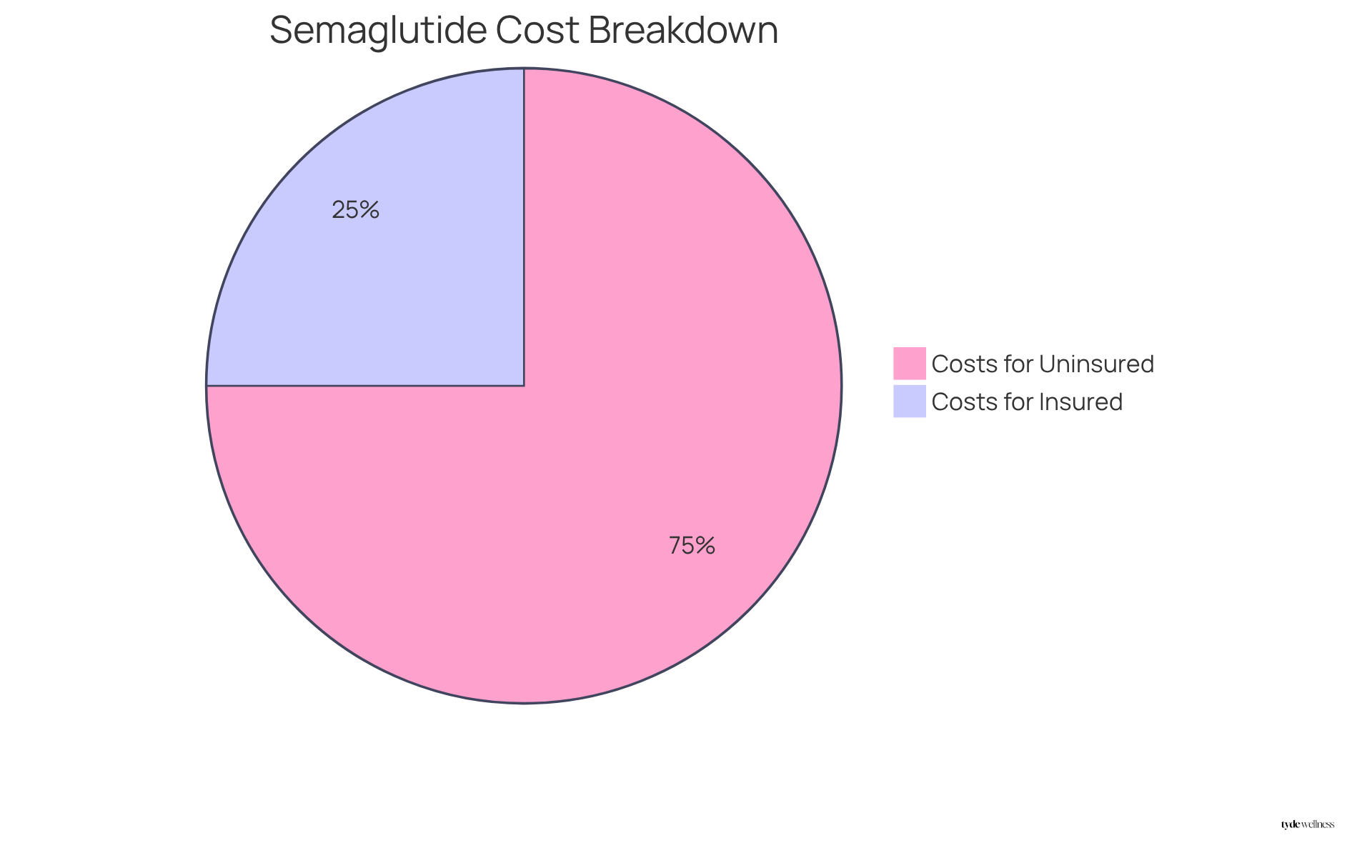
Evaluate Costs of Semaglutide With and Without Insurance
The financial environment surrounding semaglutide treatment is complex, with costs that can vary significantly based on health plan support. For individuals without coverage, the monthly cost may range from $200 to $2,000, which can impose a considerable financial burden. Conversely, those with insurance may find their expenses reduced to as low as $0, with many spending only a few hundred dollars each month, contingent upon their specific policy and benefits. Therefore, is essential; individuals should thoroughly assess their plans to gain a clear understanding of potential out-of-pocket expenses.
For instance, while some plans may cover certain medications under specific conditions, most private health insurers limit coverage of GLP-1 drugs to individuals with diabetes, thereby restricting options for those seeking weight loss treatments. Furthermore, recent updates indicate that the cost of Ozempic has been adjusted to $499 for uninsured individuals, significantly impacting the financial landscape for those considering semaglutide treatment.
At Tyde Wellness, patients have access to personalized peptide therapy and tailored GLP-1 treatment programs specifically designed for sustainable weight loss, which can be particularly advantageous for perimenopausal women. Real-world examples illustrate the financial implications: women embarking on weight loss journeys often report that health plan support can be transformative, significantly alleviating the financial strain associated with these medications. As the healthcare landscape continues to evolve, staying informed about pricing updates and coverage policies is crucial for making empowered health decisions.
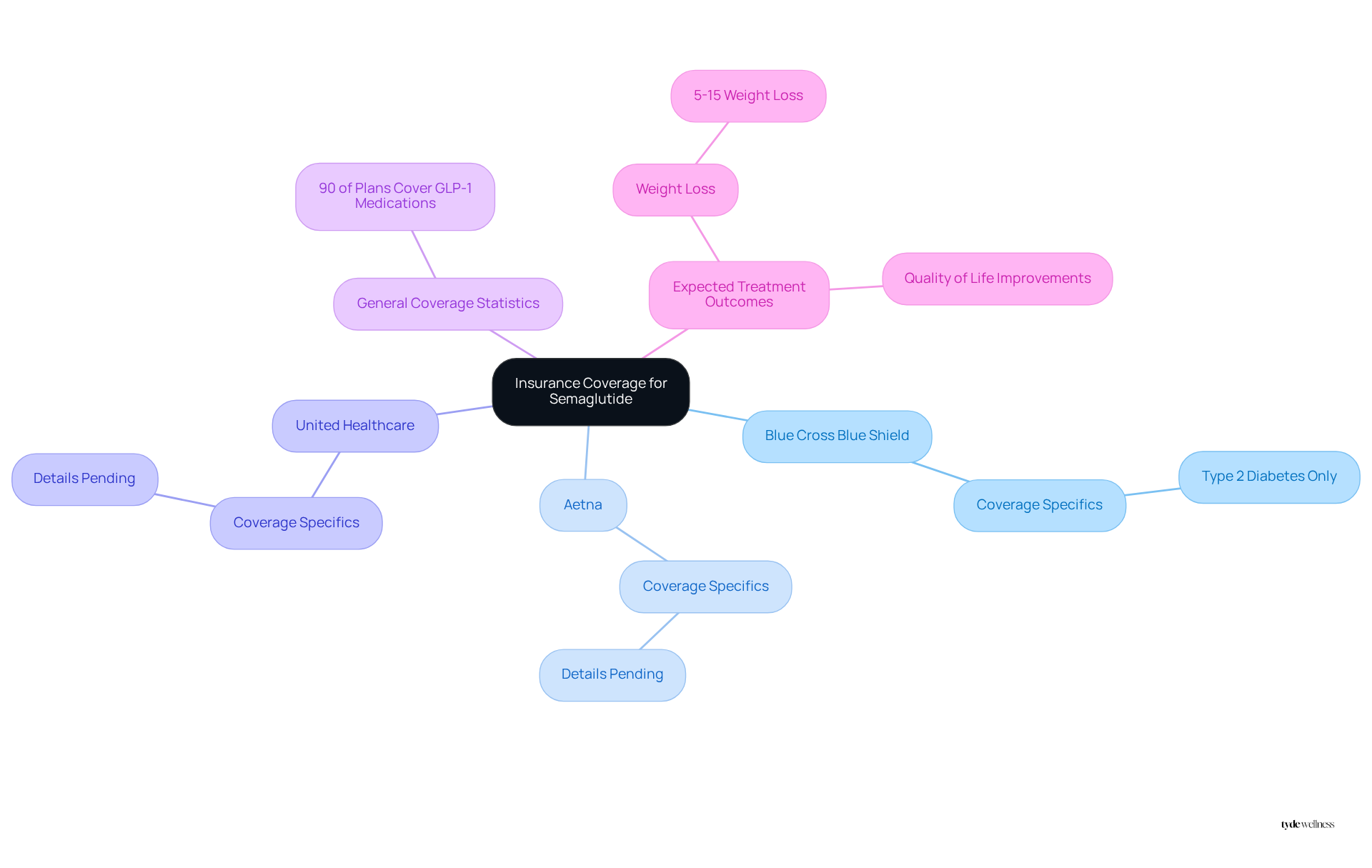
Identify Insurance Companies That Cover Semaglutide
Many firms, including prominent providers such as Blue Cross Blue Shield, Aetna, and United Healthcare, offer plans for semaglutide. However, the specifics of coverage can differ significantly among plans, making it crucial for patients to review their individual policy details. As of 2025, approximately 90% of insurance plans cover GLP-1 medications, indicating a growing acceptance of these treatments for obesity management.
Notably, Blue Cross Blue Shield Massachusetts will limit coverage for the medication to cases of type 2 diabetes starting in January 2026, raising concerns about accessibility for individuals seeking weight management solutions.
At Tyde Wellness, individuals can expect to lose 5-15% of their body weight over several months through GLP-1 therapy, nutrition coaching, and exercise, leading to improved energy levels and overall quality of life. Our team is dedicated to continuously to ensure you remain on track for success.
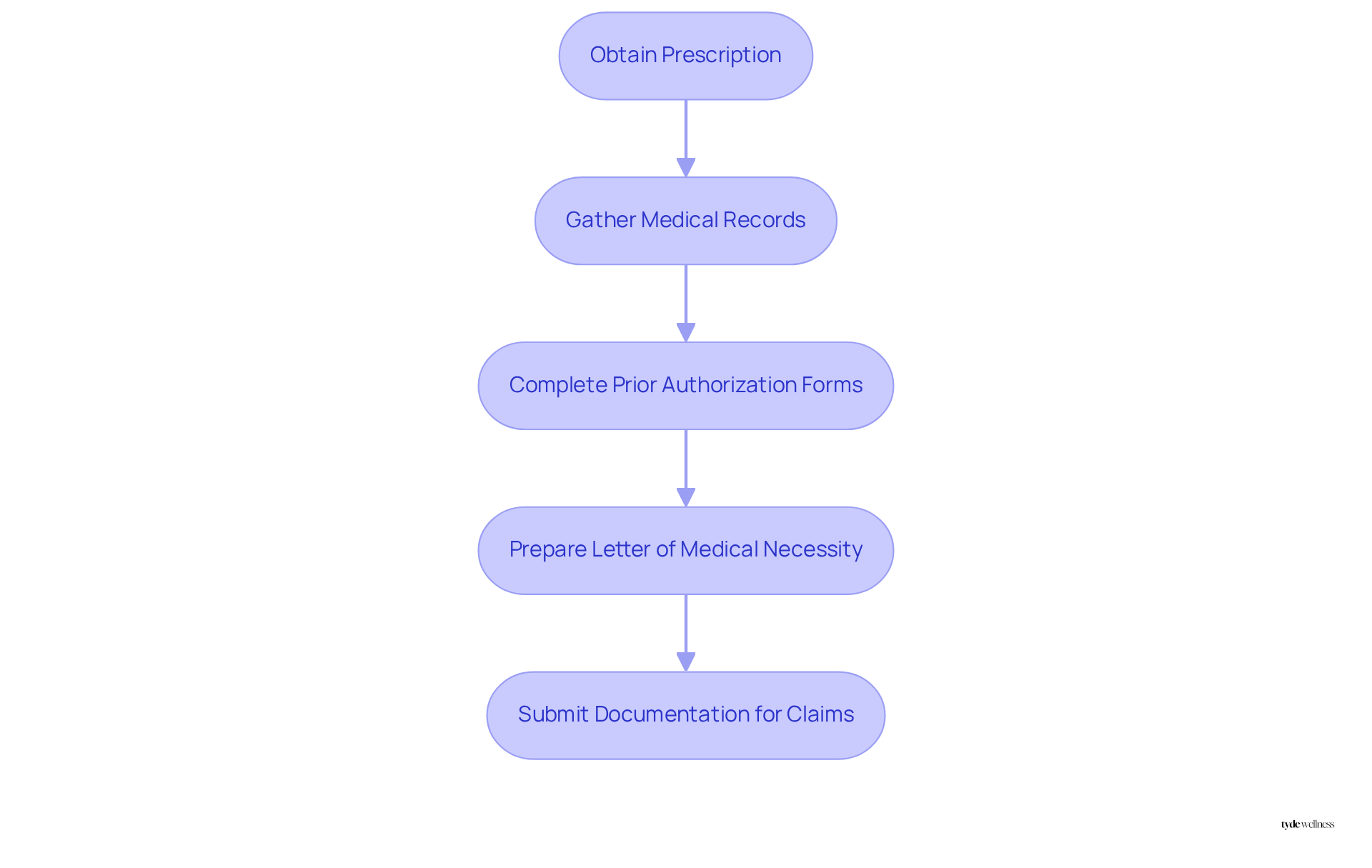
Gather Necessary Documentation for Semaglutide Insurance Claims
To effectively support insurance claims for semaglutide, patients should meticulously gather essential documentation, including:
- A prescription from a healthcare provider, confirming the medical necessity of the medication.
- Medical records that illustrate the need for treatment, including Body Mass Index (BMI) and any associated health conditions.
- Any prior authorization forms required by the provider, as these are often necessary for coverage approval.
- A letter of medical necessity from the healthcare provider, if relevant, explaining why the medication is essential for the individual’s health.
Having these documents prepared can significantly streamline the claims process, increasing the likelihood of approval. In fact, approximately 44% of insurance denials are successfully appealed, underscoring the importance of comprehensive documentation. Real-world examples demonstrate that patients who present comprehensive and well-structured information achieve higher success rates in securing coverage for the medication, especially when they include proof of previous treatment attempts and detailed medical histories.
As we approach 2025, ensuring that all essential documents are organized will be crucial, particularly since many health initiatives may require a Letter of Medical Necessity for specific prescriptions. Consulting with healthcare providers about the specifics of preparing these claims can further enhance the chances of approval.
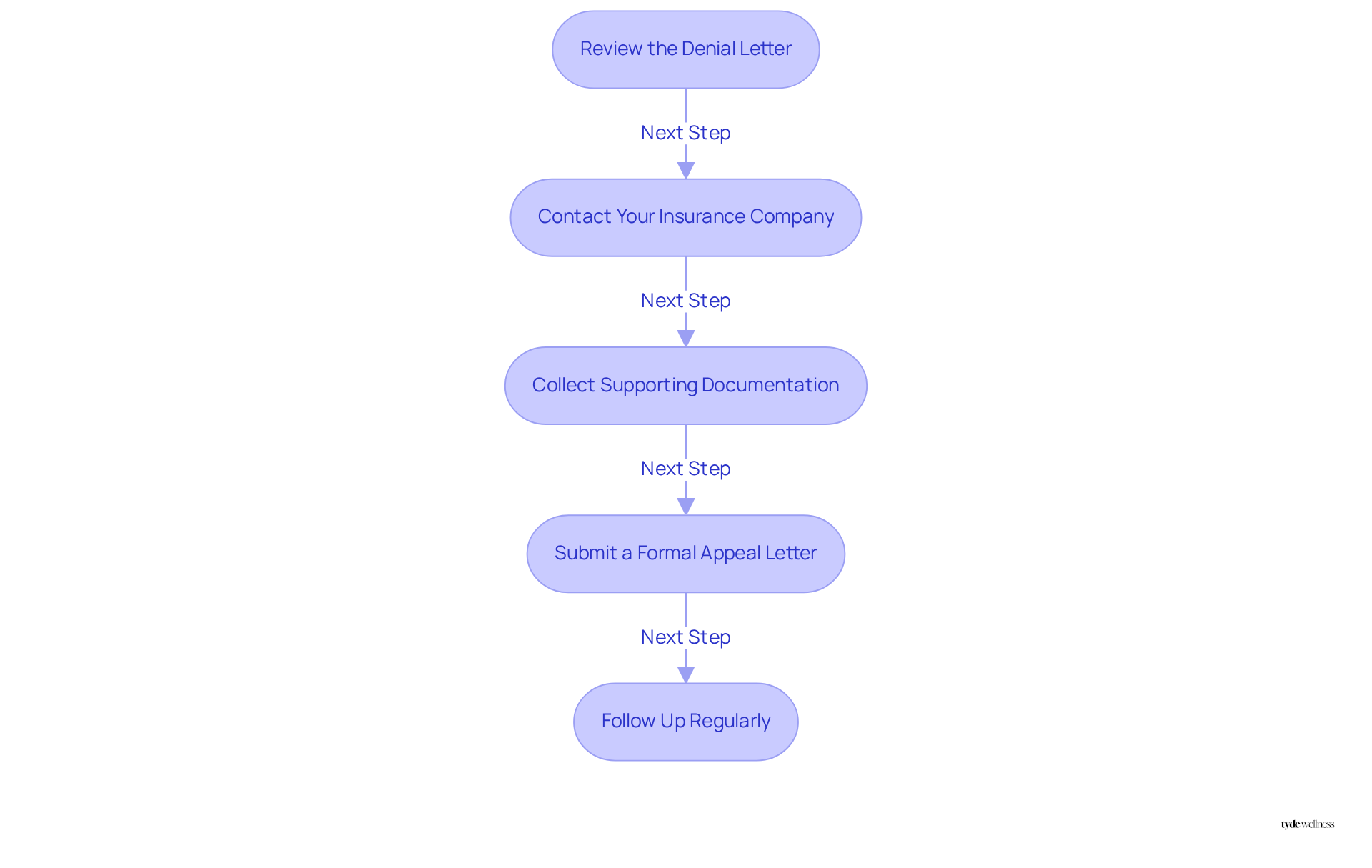
Navigate the Appeal Process for Denied Semaglutide Claims
If your insurance claim for semaglutide is denied, follow these essential steps to effectively navigate the appeal process:
- Review the Denial Letter: Understand the specific reasons for the denial. This may include claims that the medication is not medically necessary or that there is a lack of prior treatment attempts.
- Contact Your Insurance Company: Reach out to discuss the denial and gather detailed information about the appeal process. This includes any specific documentation that may be required.
- Collect Supporting Documentation: Gather additional evidence to strengthen your case. This may include medical records, a letter of from your healthcare provider, documentation of previous weight loss attempts, and relevant clinical studies that support the necessity of the medication.
- Submit a Formal Appeal Letter: Write a clear and concise appeal letter outlining your case. Include all supporting documents and explain why semaglutide is necessary for your treatment. Highlight any relevant health issues that underscore the importance of the medication, including potential health complications associated with untreated obesity.
- Follow Up Regularly: Stay in contact with your provider to ensure your appeal is being processed. It is essential to monitor timelines, as coverage plans must inform you within 10 days of receiving your appeal and come to a decision within 30 days.
Real-life experiences demonstrate that persistence yields results; approximately 44% of denials related to coverage are successfully appealed. This often occurs because weight loss medications are categorized as cosmetic rather than medical treatments. Legal experts emphasize the importance of thorough documentation and clear communication in these cases. By adhering to these steps, you can improve your likelihood of securing support for the medication and restoring your well-being.
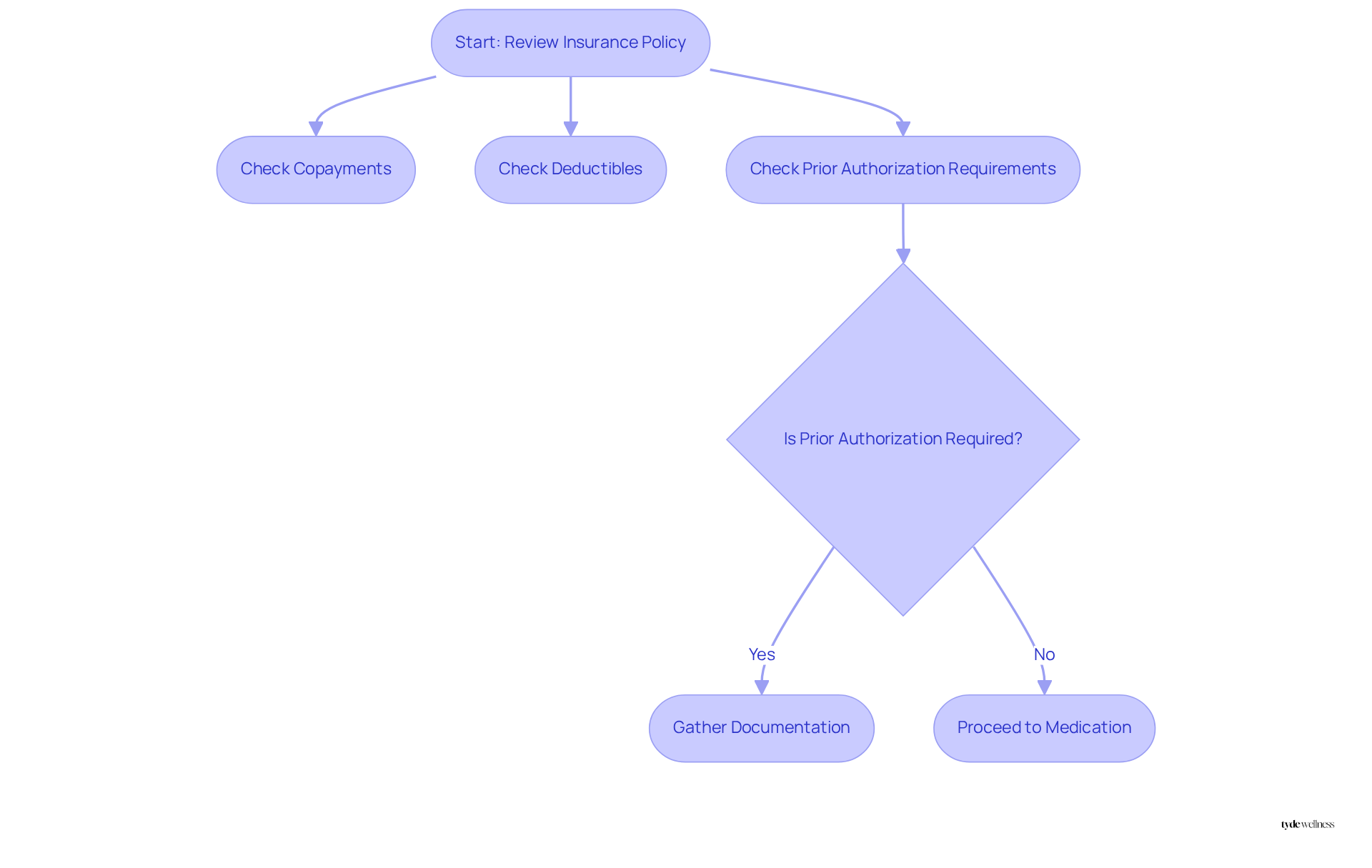
Review Your Insurance Policy for Semaglutide Coverage Details
A comprehensive examination of your insurance policy is crucial for understanding the benefits related to your medication. Focus on sections that discuss prescription drugs and weight loss therapies, emphasizing any specific requirements for inclusion. Key details to review include:
- Copayments
- Deductibles
- Prior authorization requirements
These can significantly affect your out-of-pocket costs. For instance, many insurers may require documentation of medical necessity or evidence of a trial of lifestyle changes before approving reimbursement for semaglutide.
GLP-1 medications, such as Wegovy and Ozempic, facilitate weight loss by regulating blood sugar, suppressing appetite, and reducing cravings. These features make them a valuable option when combined with a personalized nutrition and exercise plan. This preparation will empower you in and insurance company, ensuring you are well-informed about your options.
Real-world experiences indicate that women often face challenges navigating these policies, underscoring the importance of clarity in understanding benefits. As Dr. Katherine H. Saunders noted, “It’s been extremely frustrating because [Wegovy] is the most effective obesity medication we’ve ever seen and there are many insurers who won’t cover it at all.” By proactively examining your coverage details, you can better advocate for your health and secure the necessary support.
Additionally, engaging with the Tyde Circle community can offer valuable insights and encouragement as you navigate these complexities. This collective support is essential in achieving sustainable weight loss and overall wellness. As a Tyde Circle member, you also gain access to exclusive perks and discounts on Tyde Wellness programs, enhancing your journey toward better health.
Explore FAQs About Semaglutide and Insurance Coverage
Frequent inquiries regarding medication and policy support often arise as individuals seek clarity on their treatment alternatives. Key questions include:
- What steps should I take if my provider denies coverage?
- How can I confirm if my coverage plan includes semaglutide?
- What specific documentation is required for my insurance claim?
- Are there assistance programs available to help with costs?
- How frequently should I schedule follow-up appointments with my healthcare provider?
Addressing these questions enables individuals to navigate their weight loss journey with confidence. For instance, many women have found that consistent communication with their coverage providers can yield favorable outcomes, particularly when contesting coverage denials. Moreover, customer assistance programs can significantly alleviate financial burdens, with data indicating that these programs have supported thousands in accessing essential medications.
Healthcare experts emphasize the importance of understanding coverage plans and recognizing potential systemic barriers that may affect access to GLP-1 therapies. Real-life experiences shared by individuals who have successfully underscore the value of being proactive and informed. By equipping themselves with knowledge and resources, patients can more effectively advocate for their health and ensure they receive the necessary support.

Conclusion
Navigating the complexities of obtaining semaglutide coverage through insurance can be daunting. However, understanding the process significantly enhances accessibility to this vital treatment for weight management. This article outlines essential steps and strategies to ensure individuals can effectively secure coverage, emphasizing the importance of personalized consultations and thorough documentation.
Key arguments highlighted include:
- The necessity of understanding eligibility criteria
- Engaging with healthcare providers for prescriptions
- Meticulously gathering the required documentation for insurance claims
Furthermore, the appeal process for denied claims is crucial, as many individuals have successfully overturned denials by presenting compelling evidence of medical necessity and maintaining persistence in communication with insurers.
Ultimately, the journey to obtaining semaglutide coverage is not merely about navigating insurance policies; it is about empowering individuals to take charge of their health and well-being. By leveraging the insights and resources provided, individuals can advocate for themselves more effectively, ensuring they receive the support necessary for sustainable weight loss. Engaging with communities like Tyde Circle can further enhance this experience, providing encouragement and shared knowledge that can lead to successful outcomes in their health journeys.
Frequently Asked Questions
What services does Tyde Wellness offer for weight loss?
Tyde Wellness provides personalized weight loss programs that incorporate GLP-1 medication, specifically designed for women undergoing significant life changes, such as postpartum recovery and menopause. These programs focus on sustainable weight reduction strategies and include personalized nutrition plans.
How effective is GLP-1 medication for weight loss?
Research indicates that GLP-1 medication is particularly effective for weight loss, with women often reporting higher success rates when utilizing these therapies. This approach not only aids in weight management but also promotes overall well-being.
What are the eligibility criteria for semaglutide insurance coverage?
To qualify for semaglutide coverage, individuals typically need to have a body mass index (BMI) of 25 or higher, or a BMI of 27 or higher with at least one weight-related health condition, such as hypertension or diabetes.
What steps should I follow to obtain semaglutide through insurance?
The steps include: 1. Consult your healthcare provider for a prescription. 2. Verify coverage with your insurance provider. 3. Submit any required prior authorization forms. 4. Document all communications and submissions. 5. Negotiate with your provider if your request is denied. 6. Explore manufacturer assistance programs for potential cost reduction. 7. Consult insurance experts for additional guidance.
How can I verify if my insurance covers semaglutide?
You can verify coverage by contacting your insurance provider directly or using their online resources. It’s important to check as only 45% of private health plans include coverage for medications aimed at weight reduction.
What should I do if my insurance request for semaglutide is denied?
If your request is denied, you can negotiate with your insurance provider, review your policy specifics, and consider submitting a formal appeal. Many individuals have successfully reversed denials by demonstrating the medical necessity of the treatment.
Are there any support programs available for obtaining semaglutide?
Yes, assistance programs offered by manufacturers, such as Novo Nordisk, can provide semaglutide at reduced prices or even free for qualifying individuals.
List of Sources
- Tyde Wellness: Personalized Weight Loss Programs with Semaglutide Coverage
- Here’s what it would take for insurance to cover weight loss drugs (https://nbcnews.com/health/health-news/insurance-cover-weight-loss-drugs-take-rcna120091)
- Rising Costs Lead Insurers to Drop Weight Loss Drug Coverage, Further Increasing Patient Burden (https://ajmc.com/view/rising-costs-lead-insurers-to-drop-weight-loss-drug-coverage-further-increasing-patient-burden)
- Major insurance changes are coming to GLP-1 drugs for weight loss. Here’s how that could affect patients | CNN (https://cnn.com/2025/07/01/health/zepbound-wegovy-insurance-cvs-bcbs-weight-loss)
- A Real-World Study of the Effectiveness and Safety of Semaglutide for Weight Loss – PMC (https://pmc.ncbi.nlm.nih.gov/articles/PMC11144277)
- Weight Loss Outcomes Associated With Semaglutide Treatment for Patients With Overweight or Obesity – PMC (https://pmc.ncbi.nlm.nih.gov/articles/PMC9486455)
- Understand Eligibility Criteria for Semaglutide Insurance Coverage
- Insurance Coverage, Type of Employment Shape Inequities in Access to Semaglutide (https://bu.edu/sph/news/articles/2025/insurance-coverage-type-of-employment-shape-inequities-in-access-to-semaglutide)
- Are You Eligible for Ozempic? New Study Suggests Over Half of U.S. Adults Qualify (https://health.com/ozempic-semaglutide-american-eligibility-8747341)
- More than half of all US adults are eligible for semaglutide therapy (https://news-medical.net/news/20241120/More-than-half-of-all-US-adults-are-eligible-for-semaglutide-therapy.aspx)
- New eligibility for semaglutide would cost Medicare billions in spending (https://healio.com/news/primary-care/20240826/new-eligibility-for-semaglutide-would-cost-medicare-billions-in-spending)
- Follow Steps to Obtain Semaglutide Through Your Insurance
- How to Get Ozempic & GLP-1’s Covered by Insurance (or Save Big with Plum Health Direct Primary Care): The Ultimate Guide You Can’t Afford to Miss! — Plum Health Direct Primary Care (https://plumhealthdpc.com/blog/how-to-get-ozempic-covered-by-insurance-the-ultimate-guide-you-cant-afford-to-miss)
- Comprehensive Semaglutide Data & Statistics: Weight Loss & Diabetes (https://hydramed.com/rx/semaglutide/data-statistics-weight-loss-diabetes-cardiovascular-clinical-studies)
- How to get semaglutide covered by insurance (https://getheally.com/patients/news/how-to-get-semaglutide-covered-by-insurance)
- Check your Coverage for Wegovy® (semaglutide) injection 2.4 mg | NovoCare® (https://novocare.com/obesity/products/wegovy/check-coverage.html)
- Consult Healthcare Providers for Semaglutide Prescription Guidance
- Wegovy maker ends partnership with Hims & Hers (https://abcnews.go.com/GMA/Wellness/novo-nordisk-ends-collaboration-hims-discounted-weight-loss/story?id=123122046)
- Insurance Coverage, Type of Employment Shape Inequities in Access to Semaglutide (https://bu.edu/sph/news/articles/2025/insurance-coverage-type-of-employment-shape-inequities-in-access-to-semaglutide)
- Consultations for obesity drug prescriptions are way up over 2023, survey finds (https://npr.org/2024/12/12/nx-s1-5223557/consultations-for-obesity-drug-prescriptions-are-way-up-over-2023-survey-finds)
- Navigating Compounded Semaglutide: What Health Care Providers Need to Know (https://ajmc.com/view/navigating-compounded-semaglutide-what-health-care-providers-need-to-know)
- Evaluate Costs of Semaglutide With and Without Insurance
- Novo Nordisk lowers cost of Ozempic® to $499 per month for self-paying patients, in support of patient access to authentic, FDA-approved semaglutide medicines (https://prnewswire.com/news-releases/novo-nordisk-lowers-cost-of-ozempic-to-499-per-month-for-self-paying-patients-in-support-of-patient-access-to-authentic-fda-approved-semaglutide-medicines-302532208.html)
- Novo Nordisk slashes price of Ozempic in half to $499 for cash-paying, eligible U.S. patients | Fortune (https://fortune.com/2025/08/18/novo-nordisk-ozempic-wegovy-cash-price-drop)
- You can now get Ozempic for $499 if you pay in cash (https://nbcboston.com/news/national-international/novo-nordisk-ozempic-cost-cut-uninsured-patients/3792609)
- The cost of weight loss drugs is finally dropping. How low can prices go? (https://nbcnews.com/health/health-news/cost-weight-loss-drugs-wegovy-zepbound-how-low-prices-down-rcna205911)
- Semaglutide Costs With & Without Insurance (https://aol.com/much-does-semaglutide-cost-without-105700994.html?utm_source=flipboard&utm_content=topic/wegovy)
- Identify Insurance Companies That Cover Semaglutide
- Changes to insurance coverage for weight loss drugs are coming in 2025 (https://whyy.org/articles/independence-blue-cross-restrict-coverage-ozempic-weight-loss)
- Major insurance changes are coming to GLP-1 drugs for weight loss. Here’s how that could affect patients | CNN (https://cnn.com/2025/07/01/health/zepbound-wegovy-insurance-cvs-bcbs-weight-loss)
- Wegovy: When Insurance Won’t Cover Your Meds (https://webmd.com/obesity/features/wegovy-insurance-cover-meds)
- GLP-1 roadblocks: Discontinuation rates soar as insurers clamp down (https://pharmavoice.com/news/glp-1-roadblocks-discontinuation-rates-insurance/752252)
- Coverage and Prior Authorization for Semaglutide and Tirzepatide in Medicare Part D (https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2838260)
- Gather Necessary Documentation for Semaglutide Insurance Claims
- How to get semaglutide covered by insurance (https://getheally.com/patients/news/how-to-get-semaglutide-covered-by-insurance)
- Appealing Wegovy denial: Prior authorization, letters, and tips (https://medicalnewstoday.com/articles/drugs-how-to-appeal-wegovy-denial)
- Is Semaglutide HSA Eligible? Verify Your Coverage Today – Tyde Wellness (https://tydewellness.com/learn/is-semaglutide-hsa-eligible-verify-your-coverage-today)
- Factors Associated With Semaglutide Initiation Among Adults With Obesity – PMC (https://pmc.ncbi.nlm.nih.gov/articles/PMC11751746)
- Improving access and affordability to high-cost weight management drugs (https://cvshealth.com/news/pbm/improving-access-and-affordability-to-high-cost-weight-management-drugs.html)
- Navigate the Appeal Process for Denied Semaglutide Claims
- Insurance denials for popular new weight loss medications leave patients with risky choices | CNN (https://cnn.com/2024/01/08/health/weight-loss-drug-insurance-denials)
- Appealing Wegovy denial: Prior authorization, letters, and tips (https://medicalnewstoday.com/articles/drugs-how-to-appeal-wegovy-denial)
- Wegovy Health Insurance Denial | Law Offices of Scott Glovsky (https://scottglovsky.com/insurance-bad-faith/health-insurance-claim-denials/wegovy-health-insurance-denial)
- Denied by Insurance? A Pharmacist Tells You How to Appeal (https://t1dexchange.org/denied-by-insurance-a-pharmacist-tells-you-how-to-appeal)
- How to Appeal Wegovy Coverage Denial – NowPatient (https://nowpatient.com/blog/how-to-appeal-wegovy-coverage-denial)
- Review Your Insurance Policy for Semaglutide Coverage Details
- Rising Costs Lead Insurers to Drop Weight Loss Drug Coverage, Further Increasing Patient Burden (https://ajmc.com/view/rising-costs-lead-insurers-to-drop-weight-loss-drug-coverage-further-increasing-patient-burden)
- How US commercial health plans are covering semaglutide (Wegovy®) for obesity management – Center for the Evaluation of Value and Risk in Health (https://cevr.tuftsmedicalcenter.org/news/how-us-commercial-health-plans-are-covering-semaglutide-wegovy-for-obesity-management-2)
- Insurance Coverage, Type of Employment Shape Inequities in Access to Semaglutide (https://bu.edu/sph/news/articles/2025/insurance-coverage-type-of-employment-shape-inequities-in-access-to-semaglutide)
- Wegovy: When Insurance Won’t Cover Your Meds (https://webmd.com/obesity/features/wegovy-insurance-cover-meds)
- Weight-loss patients taking Zepbound forced to switch to Wegovy after drop in coverage (https://foxnews.com/health/weight-loss-patients-taking-zepbound-forced-switch-wegovy-after-drop-coverage)
- Explore FAQs About Semaglutide and Insurance Coverage
- Insurance Coverage For Ozempic, Zepbound Went Down In 2025 (https://forbes.com/sites/brucelee/2025/03/21/insurance-coverage-for-ozempic-zepbound-went-down-in-2025)
- Insurance Coverage, Type of Employment Shape Inequities in Access to Semaglutide (https://bu.edu/sph/news/articles/2025/insurance-coverage-type-of-employment-shape-inequities-in-access-to-semaglutide)
- Live Updates: Insurance Coverage for GIP and GLP-1 Agonists Like Zepbound & Wegovy in 2025 – GoodRx (https://goodrx.com/healthcare-access/research/tracking-insurance-coverage-weight-loss-meds?srsltid=AfmBOoq4jwHVMyM8UjFf62gFMeKsjP9D0LmEBXD3Wih5unwM-PpHw2tH)
- Major insurance changes are coming to GLP-1 drugs for weight loss. Here’s how that could affect patients | CNN (https://cnn.com/2025/07/01/health/zepbound-wegovy-insurance-cvs-bcbs-weight-loss)
- How US commercial health plans are covering semaglutide (Wegovy®) for obesity management – Center for the Evaluation of Value and Risk in Health (https://cevr.tuftsmedicalcenter.org/news/how-us-commercial-health-plans-are-covering-semaglutide-wegovy-for-obesity-management-2)


